What are superbugs?
Superbugs are, simply put, common bacteria that have become resistant to various antibiotics. In other words, they are germs that can no longer be eliminated with the usual medications used to treat their infections. This means that antibiotics that used to kill those bacteria are now ineffective, making it much harder to cure the infections they cause.
When a bacterium becomes a superbug, the diseases it causes stop responding to first-line treatments. This can lead to infections that were once easy to cure becoming dangerous, with a higher risk of complications and even death. For example, a urinary tract infection, pneumonia, or surgical wound infection caused by a superbug can become prolonged and worsen because normal antibiotics no longer work.
To understand it better, below we see some differences between a common bacterium and a superbug:
| Aspect | Infection by common bacterium | Infection by superbug |
|---|---|---|
| Response to treatment | Responds to usual antibiotics that manage to eliminate it. | Does not respond to common antibiotics; stronger or specific medications are required (and sometimes there are no effective options). |
| Ease of treatment | Can be easily treated with a suitable antibiotic. | Difficult to treat: may require combinations of drugs, longer treatment time, and close monitoring. |
| Risk to the patient | Low: the infection usually cures without complications when treated correctly. | High: the infection may become prolonged, cause serious complications, and even be fatal if no effective treatment is found. |
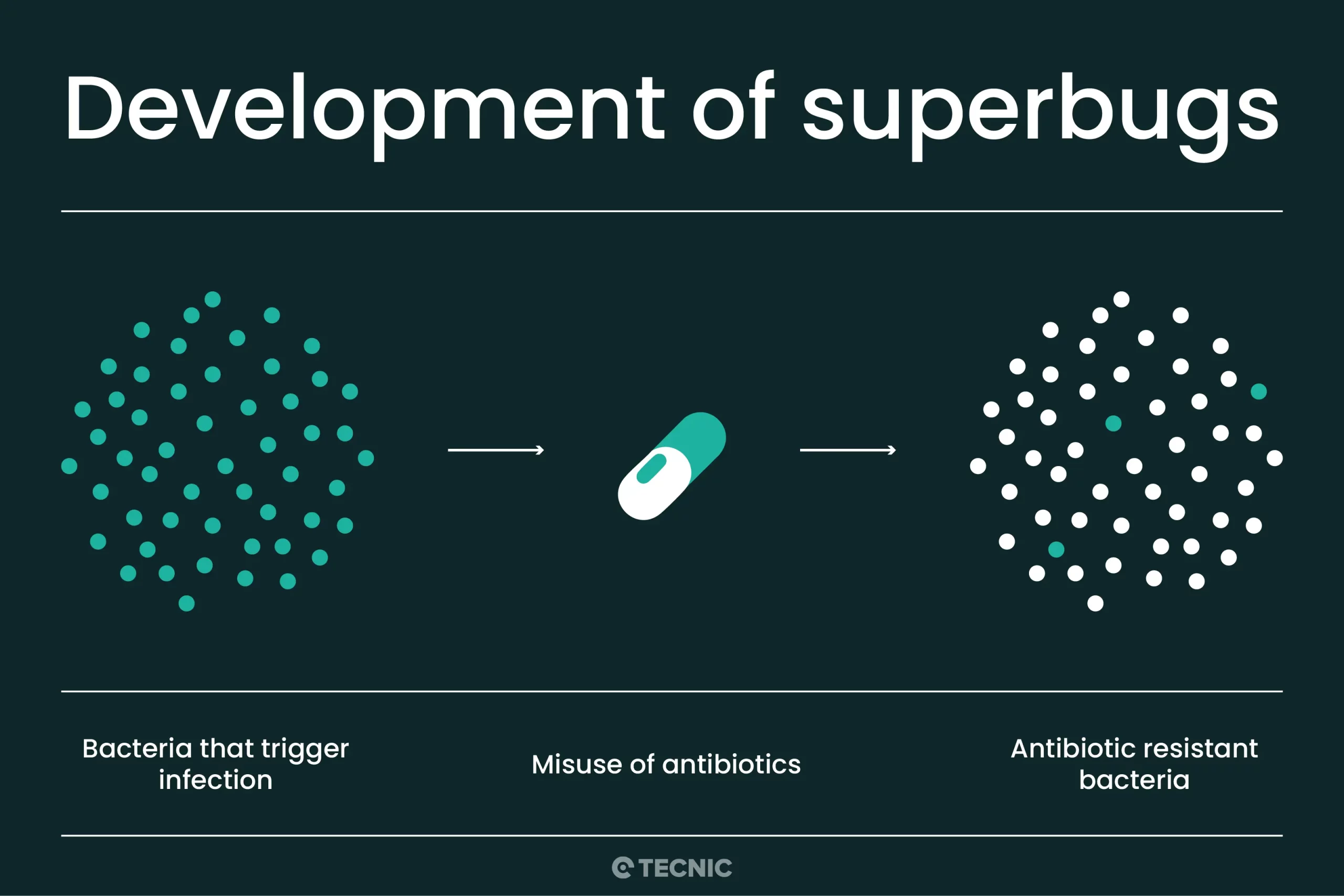
How are superbugs created?
Bacterial resistance to antibiotics is partly a natural process, the result of mutations and evolution, but the misuse of antibiotics in humans and animals is accelerating this process. Simply put: every time we use an antibiotic, we give bacteria the chance to become stronger. If the antibiotic is not used properly, bacteria "learn" to resist it. Over time, they can develop defenses that make them immune to that drug and sometimes to several others.
There are several practices that contribute to the creation of superbugs:
- Improper use in people: Taking antibiotics when not needed, for example to treat colds or flu (which are caused by viruses), is useless against the virus and instead can kill beneficial bacteria and favor the survival of resistant bacteria. Also, not completing the full treatment or self-medicating with "leftover" antibiotics are risky practices. If the antibiotic is stopped halfway through an infection, the weaker bacteria die, but the stronger ones may survive and become resistant. Similarly, using pills left over from another time or taking a random antibiotic (without medical diagnosis) may be useless against the current bacterium and promote resistance.
- Use in livestock and agriculture: A large proportion of antibiotics worldwide are used in farm animals to promote growth or prevent diseases. This extensive use (sometimes unnecessary) in livestock contributes to the emergence of resistant bacteria that can then be transmitted to humans through food, water, or the environment. In fact, most antibiotics are not used in human patients, but in animals, which also impacts resistance.
- Person-to-person transmission: Superbugs do not only emerge inside the body of someone who misuses antibiotics. They can also spread. For example, if a person carries a resistant bacterium (due to previous misuse of antibiotics or contagion in a hospital), they can transmit it to others just like any normal bacterium. Thus, superbugs are transmitted between people, animals, and the environment, spreading resistance genes. That's why the misuse of antibiotics in one individual can end up affecting the entire community.
In short, the perfect formula to create superbugs occurs when antibiotics are used excessively or incorrectly. The way we have used these drugs is helping to create new resistant superbugs. Each inappropriate use (insufficient dose, interrupted treatment, unnecessary use) is an opportunity for some bacteria to survive, adapt, and become harder to kill.
Why are they a public health problem?
Superbugs represent a serious challenge for global public health. In fact, the World Health Organization (WHO) warns that antibiotic resistance is one of the biggest threats to global health today. Why? Because we are increasingly seeing common infections that no longer respond to treatment. Diseases such as pneumonia, tuberculosis, gonorrhea, or foodborne infections from Salmonella, which used to be easily curable, are now harder, and sometimes impossible, to treat as antibiotics lose effectiveness.
The consequences of this situation are worrying:
- More deaths and complications: When an antibiotic doesn't work, the infection can worsen. It is estimated that in 2019 around 1.3 million deaths worldwide were directly caused by antibiotic-resistant infections, and up to 5 million deaths were related to antimicrobial resistance overall. This surpasses, for example, annual deaths from HIV/AIDS, giving an idea of the magnitude of the problem. Every year, thousands of people die from infections that no longer respond to any effective drug.
- Longer hospital stays and higher costs: People with superbug infections tend to stay longer in hospitals, require more intensive care, and more expensive alternative treatments. All this increases medical costs and burdens health systems. A patient who could have been treated at home with pills, if infected by a superbug, may end up spending weeks in the hospital on strong intravenous antibiotics.
- Risk to medical procedures: Many procedures we take for granted (surgeries, chemotherapy, transplants, complicated births) depend on antibiotics working to prevent or treat infections. If superbugs proliferate, routine medical procedures could become much more dangerous due to the risk of untreatable infections. The WHO and other organizations fear a scenario where we return to the pre-antibiotic era, when currently minor infections could be deadly due to lack of effective treatment.
Examples of known superbugs
Some superbugs have become sadly famous for their dangerousness. In fact, the U.S. Centers for Disease Control and Prevention (CDC) have identified several resistant bacteria considered urgent threats to health. Among the best-known superbugs are:
- MRSA (Methicillin-resistant Staphylococcus aureus): a variety of the bacterium Staphylococcus aureus that has developed resistance to penicillin-type antibiotics (like methicillin and oxacillin). MRSA can cause skin infections, pneumonia, and serious wound or blood infections, especially in hospital settings. It used to be treated with common antibiotics, but now these infections require stronger medications and are much harder to manage.
- Carbapenem-resistant Enterobacteriaceae (CRE): this group includes intestinal bacteria like Escherichia coli or Klebsiella pneumoniae that have become resistant to carbapenems, some of the most powerful antibiotics available. CRE can cause urinary tract infections, pneumonia, or very complicated sepsis, since practically no standard antibiotic eliminates them. Some produce enzymes (like ESBL or NDM) that deactivate many antibiotics. These superbugs are especially dangerous in hospitals, where they can cause difficult-to-control outbreaks.
- Vancomycin-resistant Enterococcus (VRE): Enterococcus is a bacterium that usually lives in the intestine. Certain strains have developed resistance to vancomycin (a last-resort antibiotic). VRE can cause urinary, wound, or blood infections that are complex to treat, especially in weakened patients. Being resistant to one of the strongest antibiotics forces the use of less effective or more toxic options.
- Multidrug-resistant Neisseria gonorrhoeae: the bacterium that causes gonorrhea, a sexually transmitted disease, has become resistant to almost all antibiotics traditionally used to treat it. Today there are strains of gonorrhea for which only one or two effective antibiotics remain, and some nearly untreatable ones have already been detected. This is alarming because gonorrhea can cause serious complications (infertility, systemic infections) if left uncured.
- Drug-resistant Mycobacterium tuberculosis: the tuberculosis bacterium has developed multidrug-resistant (MDR-TB) and extensively drug-resistant (XDR-TB) strains. TB is a serious lung infection that, in its resistant form, requires very prolonged treatments (up to 2 years) with combinations of specialized drugs, and even then cure rates are lower. Drug-resistant TB is a major public health problem in several regions of the world.

How are superbugs fought?
A logical question is whether being infected with a superbug equals a hopeless situation. The good news is that many infections caused by superbugs can indeed be treated, although with more complexity. The bad news is that the more resistant the bacterium, the fewer treatment options are available.
In practice, when a bacterium is resistant to the first-choice antibiotic, other stronger or less common antibiotics are used. For example, certain infections resistant to penicillins can be treated with vancomycin; and if they are also resistant to that, perhaps with linezolid or daptomycin, etc. However, these “last-line” drugs are usually more toxic, more expensive, and less effective than common antibiotics. This means the patient may experience more side effects and that treatment success is not 100% guaranteed.
What happens if the bacterium is resistant to all known antibiotics?
In rare cases, infections have been found caused by practically untreatable (pan-resistant) bacteria. In such situations, doctors may try unusual combinations of several drugs at once, use higher doses (with a high risk of toxicity), or resort to alternative experimental therapies. One of them is bacteriophage therapy, which uses specific viruses that infect and destroy bacteria; another line of research is new antibiotics or boosting the patient’s immune system to control the infection. However, as of today, if a superbug does not respond to any antibiotic, the options are extremely limited and the prognosis may be very serious.
At a global level, the scientific community and health authorities are fighting on two fronts: on the one hand, promoting the proper use of current antibiotics (to prolong their effectiveness), and on the other hand, developing new drugs. Developing a new antibiotic is a long (10–15 years) and costly process, and in recent decades very few novel antibiotics have reached the market. This means that, at the pace bacteria develop resistance, the number of effective drugs is falling short. That’s why there is so much emphasis on preserving the antibiotics that still work. International initiatives such as the WHO’s “World Antimicrobial Awareness Week” aim to educate about this issue and promote responsible use policies.

What can the public do to stop superbugs?
Although the resistance problem may seem enormous, we can all help prevent it with very specific actions in our daily lives. Antibiotic resistance will not stop entirely (since bacteria always evolve), but we can slow it down significantly. Here are some preventive measures and good practices that the general public can adopt:
- Use antibiotics only when necessary and prescribed: Antibiotics only work against bacterial infections, not against viruses like flu or colds. Don’t insist on a prescription if your doctor says it’s unnecessary. Never self-medicate with antibiotics or use leftovers from a previous treatment. If the doctor prescribes you an antibiotic, follow the instructions exactly: correct dosage and complete the full course, even if you feel better before finishing. This ensures all bacteria are eliminated and no resistant survivors remain.
- Hand and personal hygiene: Washing your hands well with soap and water frequently is one of the most effective ways to prevent all kinds of infections. Wash especially before eating, after using the bathroom, and when returning home. If soap and water are unavailable, use alcohol-based hand gel. Maintaining good personal and environmental hygiene (e.g., cleaning and disinfecting surfaces at home when someone is sick) reduces the spread of germs, including resistant bacteria.
- Food safety: Handle and cook food properly. Wash fruits and vegetables, cook meat thoroughly (especially chicken and ground meat) to kill bacteria, and avoid cross-contamination by using different cutting boards/knives for raw meat and vegetables. Resistant bacteria can also come through food, so good food hygiene keeps them at bay.
- Avoid contagion: Many infections (including resistant ones) spread from person to person. Cover your mouth when coughing or sneezing, stay home if you have a contagious infection to avoid exposing others, and keep your vaccinations up to date (e.g., flu, pneumococcal vaccine, etc., which prevent secondary bacterial diseases). For sexually transmitted infections, use condoms for protection—resistant gonorrhea is prevented the same way as non-resistant strains, by avoiding risky behavior.
- Vaccination: Getting vaccinated doesn’t act directly on resistant bacteria, but it’s a key strategy to prevent infections. Many vaccines protect us from bacterial diseases (diphtheria, whooping cough, pneumococcal pneumonia, tuberculosis in certain countries, etc.), preventing the need to use antibiotics in the first place. Fewer infections = fewer antibiotics prescribed = fewer chances for superbugs to emerge. Even vaccines against viruses (e.g., flu, COVID-19) help indirectly by preventing secondary bacterial complications usually treated with antibiotics. Keeping your vaccination schedule up to date protects you and reduces the circulation of pathogens in the community.
In short, prevention depends on healthy personal habits and conscious antibiotic use. Each individual, with small actions, contributes to the fight against superbugs. The WHO emphasizes that it is urgent to change how we use these medications and to adopt hygiene, vaccination, and precautionary measures to reduce the spread of infections. This way we protect the effectiveness of antibiotics for ourselves and future generations.
Conclusion
Superbugs are a major challenge but not an invincible one. Understanding what they are and how they originate allows us to take action: use antibiotics wisely, maintain hygiene, and support public health measures. Health authorities around the world are calling for shared responsibility in combating this problem. If everyone does their part, doctors, patients, farmers, governments, we can stop superbugs and continue to benefit from antibiotics for many years to come. The fight against resistance is everyone’s task, and every small action counts. Humanity’s health in the future may depend on the decisions we make today.
Frequently Asked Questions (FAQ)
A superbug is a bacterium that has become resistant to multiple antibiotics, making it difficult or impossible to treat.
They are mainly caused by the overuse or misuse of antibiotics in humans, animals, and agriculture.
You can get infected through contact with contaminated surfaces, people, hospitals, or food containing resistant bacteria.
MRSA (Methicillin-resistant Staphylococcus aureus) is one of the most well-known superbugs.
Yes, but they may require powerful or less common antibiotics, and in some cases, there may be no effective treatment available.
References
Centers for Disease Control and Prevention (CDC). (2019). Antibiotic Resistance Threats in the United States, 2019. U.S. Department of Health and Human Services.
World Health Organisation (WHO). (2020). Antimicrobial resistance.
European Centre for Disease Prevention and Control (ECDC). (2022). Antimicrobial resistance in the EU/EEA.
World Health Organization (WHO). (2022). Global Antimicrobial Resistance and Use Surveillance System (GLASS) Report 2022.
Review on Antimicrobial Resistance. (2016). Tackling Drug-Resistant Infections Globally: Final Report and Recommendations.